Cartilage has no blood vessels or nerves and is believed, by many, to be an inert tissue that does not have the ability to repair itself or adapt.
I think it is also fair to say that, for quite some time, the common belief that has been held by the general public and even some health care practitioners, is that ‘wear and tear’ of articular cartilage leads to osteoarthritis (OA).
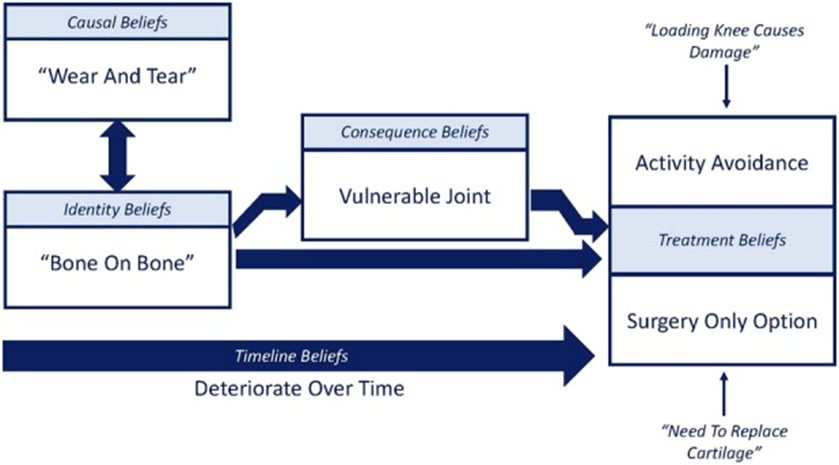
When one starts to look deeper into the available objective evidence regarding OA, it becomes evident that these beliefs are not entirely accurate. Though, as with all things in the musculoskeletal world, there is still a lot of uncertainty and unknowns.
Let’s look at some research literature and some ongoing research that sheds some doubt on these two commonly held beliefs, namely that cartilage does not have the ability to repair itself and that ‘wear and tear’ is the primary cause of OA.
Running Models vs. Real Life
When you use the known properties of cartilage and the forces of running, most models have the cartilage of knees failing at a much higher rate, and at a much younger age than what happens in real life.
Thereare studies that have compared groups of runners and non-runners over the course of decades, and found no evidence that runners are more likely to develop knee osteoarthritis.2,3,4
This is one of a few reasons that initially led to researchers postulating that cartilage is not so inert of a tissue after all, and that it can respond positively to load.
More recently, a group at the University of British Columbia performed a systematic review and meta-analysis on the influence of running on lower limb cartilage. They concluded “moderate evidence suggests that running does not lead to the formation of new lesions. Cartilage recovers well from a single running bout and adapts to repeated exposure.”5
So not only has running been proven to not wear out our joints, but it also looks like it may even stimulate adaptations that increase the health of our joints.
Mechanical Forces Are Not Irrelevant
Some fascinating ongoing research is being carried out by Professor Tonia Vincent at the Kennedy Institute of Rheumatology which is at the University of Oxford. She studies articular cartilage and its role in the pathophysiology of OA. Through her 20 years of study, she and others have confirmed that cartilage does indeed have the ability to adapt to the mechanical loads placed on it.
More specifically, she has found that growth factors, which live in the pericellular matrix surrounding a chondrocyte (a cartilage cell), react to mechanical stimuli. These growth factors can stimulate signalling pathways that result in cartilage repair.
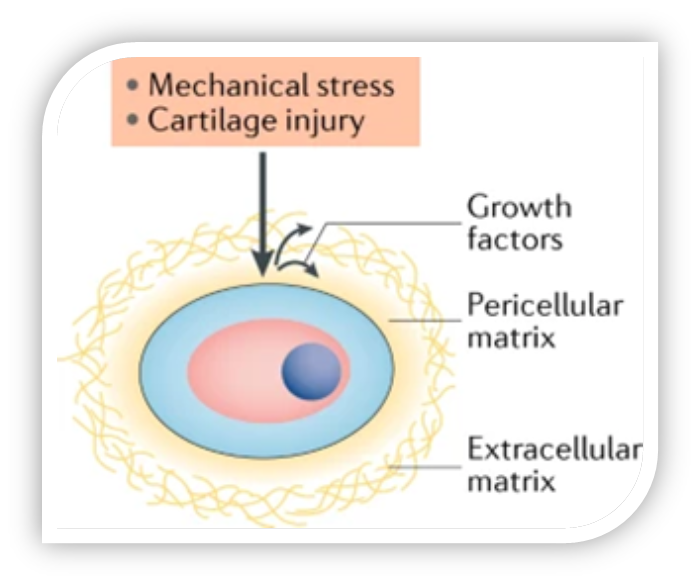
Professor Vincent is currently hypothesizing that compression forces trigger positive adaptations in the cartilage, while shear forces trigger negative responses in the cartilage.7 This is simply a postulation at this point, it will be fascinating to see what she and her team find in the years ahead.
Professor Vincent does admit that it is difficult to measure shear forces in joints and thus quantify which exercises are providing more compression than shear. She adds that there is still much work left to do with applying these findings to living humans but is encouraged at the progress that has been made thus far.
Benefits Of Exercise For OA
Perhaps the question of ‘what exercises create positive adaptations in cartilage?’ can be partially answered by the immense amount of research showing that basically all forms of exercise are beneficial for those with OA!
Professor Vincent might think I am oversimplifying things with this logic, but the movement optimist/critical thinker in me can’t help it.
Allow me to highlight just a few of the many pieces of research below:
- There is a significant amount of research evidence to show significant benefits of exercise over no exercise in people with OA.8
- High-quality evidence indicates that land-based therapeutic exercise provides reduced knee pain, and moderate quality evidence shows improvement in physical function among people with knee OA.9
- As a result of all the research showing significant benefit, exercise is recommended as the first-line treatment for OA.10
- There is not a significant difference in effect between the different types of land-based exercise interventions.11
- Stationary Cycling for Knee OA relieves pain and improves sport function in individuals with knee osteoarthritis.12
- The effects of aquatic-based exercise on symptoms and impairments are smaller than the effects of land-based exercise. However, this intervention can be very effective for those who find land-based exercise too painful.11
All these recommendations and positive research findings exist, yet many people believe that exercise will ‘wear out’ their joints and thus they avoid one of the primary things (exercise/movement) that could be helping their joints!
I am going to keep the focus of this blog on raising your awareness to the fact that OA is not solely a ‘wear and tear’ condition. Care and management of people with OA is another subject unto itself.
If you have a yearning for more knowledge regarding exercise prescription for those with OA, I cover this and more in my course → Exercise & Movement Rx – in – Modern Clinical Practice.
If you are dealing with OA yourself and are looking for a great resource to get started, look no further than Greg Lehman’s great website full of informative videos: OA Optimism.
Another factor to consider is that exercise could be helping people with OA in more ways than just stimulating positive adaptations in the cartilage. Perhaps it is increasing the strength of muscles surrounding the affected joint(s) which would help reduce the load on the passive structures in the joint(s). This increased strength could also reduce the shear forces on the joint which are hypothesized to stimulate negative adaptations in cartilage.
To look at this through a biopsychosocial lens, perhaps the exercise is connecting someone socially with other people which has been shown to have positive effects on someone’s health (ex/a regular golfing group).
Another important biological way that exercise could be helping people with OA is via its anti-inflammatory effects. We will expand on this in more detail when discussing the multifactorial nature of OA.
Multifactorial Inflammatory Condition
As with all cells, tissues, and organs in the human organism, there are many factors simultaneously interacting to influence the health of our cartilage. Osteoarthritis is considered by the leaders in the field to be an inflammatory condition with many potential causes/contributors versus solely a ‘wear and tear’ condition.
The diverse nature of the primary risk factors (genetic predisposition, aging, obesity, acute physical trauma) for developing OA suggest that that there are multiple pathways to the disease. Mechanical forces, metabolic factors, inflammatory mediators, and genetics all have been shown to play a part in the initiation and perpetuation of OA.13
The inflammatory mediators involved in Osteoarthritis can be released locally from cartilage, bone, and synovium. One of the primary causes of this release is acute trauma, such as a major sport injury like an ACL rupture.
Mechanical forces are not irrelevant. They are probably just not relevant in the way that most people believe them to be. Though I suppose one could classify a ruptured ACL as ‘wear and tear’. 😉
Remember, moderate levels of ‘loading’ through physical activity can create positive adaptations in cartilage tissue and has been shown to decrease pain and increase function in those with OA. Not to mention the secondary benefits of physical activity and exercise which are effective in preventing at least 35 chronic conditions and treating at least 26 chronic conditions.11
In addition, the inflammatory mediators can be systemic and released from tissues elsewhere in the body, carried via blood and delivered to joints via subchondral bone vasculature.14 One of the primary tissues involved in this process is adipose tissue.
It follows that obesity is one of the primary risk factors in the development of OA.15
Obesity is one example of metabolic triggered inflammation (Meta-inflammation), induced by nutrient overload and metabolic surplus. I am choosing not to get too detailed in the pathophysiology of these metabolic inflammatory processes, but the following figure is informative for those who are keen.
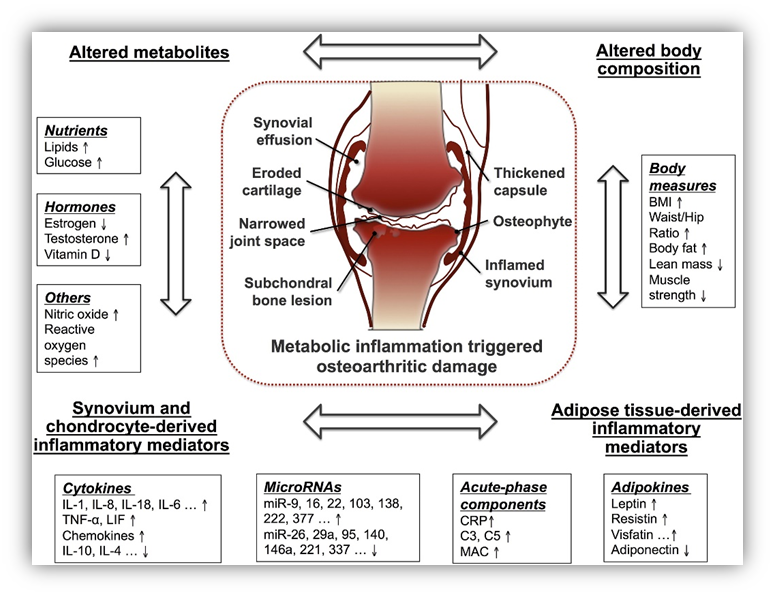
Insulin-resistance, lipid abnormalities and hypertension can also stimulate meta-inflammation mediators to be released into the blood. These inflammatory mediators cause harm/damage to joint tissues, thus initiating and/or perpetuating the OA process.14
There are more sources of inflammatory mediators that are linked with the initiation and perpetuation of OA, like aging and post-menopausal estrogen levels. I will leave it to you to explore the references cited in this section for a more detailed discussion.
Let us return to our discussion of the positive effects of exercise for those dealing with OA. Exercise is a physiological ‘stressor’ that is capable of inducing adaptations in nearly all cells, tissues, organs, and systems.
We already discussed how the mechanical forces from exercise and movement can stimulate signalling pathways that promote positive adaptations in cartilage.
Exercise is also able to help those with OA through its anti-inflammatory effects. These anti-inflammatory effects can be both direct (release of ant-inflammatory substances after each bout of exercise) and indirect (by improving physical capacity, body composition, comorbidities, and cardiovascular risk factors).17
Exercise has also been proven to decrease the concentration of proteins and compounds in our knees that are hostile to cartilage health (eg. COMP) as well as increase the concentrations of ‘cartilage-protective’ substances (eg. Interleukin-10).18,19
As we look deeper into Osteoarthritis, it becomes evident that the simplistic ‘wear and tear’ view of the condition is inaccurate and could be detrimental to the implementation of effective management of OA.
Why Stop At Cartilage?
Why stop at questioning the ‘wear and tear’ theory in relation to cartilage? Why not look at other tissues/structures that were long thought to be victims of the ‘wear and tear’ villain? How about intervertebral discs?
In a recent study it was found that “degree of physical inactivity as measured over a time period of 14 years demonstrated a strong correlation with disc degeneration of the thoracic and lumbar spine.”20
In other words, they found the less physically active someone was, the more disc degeneration they had! More support for using movement to stimulate positive adaptations in the tissues of our bodies.
Summary
The best way to summarize a long, text-heavy blog…bullet points!
- Cartilage is not an inert tissue. It is an incredibly responsive and adaptive tissue.
- Not only is it safe to ‘load’ joints (including those with osteoarthritic changes), but it is also beneficial.
- All types of exercise/movement are beneficial for OA.
- Osteoarthritis is a multifactorial inflammatory condition not solely a ‘wear and tear’ condition.
- Mechanical forces are not irrelevant. Previous acute trauma to a joint is a primary risk factor for OA.
- OA can improve and may not need surgery.

When I sat down to write this blog, I was hoping to provide a modern and evidence-based summary on some important aspects of Osteoarthritis. My goal is for this information to reach people who have erroneous and unhelpful beliefs regarding ‘loading’ and its effects on the health of articular cartilage and joints.
Let’s spread knowledge. Let’s get people dealing with OA moving at a tolerable level for them. Let’s help them to find some activity or movement or exercise that makes them feel good, is fun and is going to get done! Let’s support them so that the movement is consistently performed over a long period of time.
Thank you for reading and I encourage you to please share this blog with family, friends, and other health care professionals.
References
- Bunzli, S., O’Brien, P., Ayton, D., Dowsey, M., Gunn, J., Choong, P., & Manski-Nankervis, J. A. (2019). Misconceptions and the Acceptance of Evidence-based Nonsurgical Interventions for Knee Osteoarthritis. A Qualitative Study. Clinical orthopaedics and related research, 477(9), 1975–1983. https://doi.org/10.1097/CORR.0000000000000784
- Chakravarty, E., Hubert, H., Lingala, V., Zatarain, E., Fries, J. (2008). Long distance running and knee osteoarthritis. A prospective study. Am J Prev Med., 35(2):133-8. doi: 10.1016/j.amepre.2008.03.032.
- Lo, G., Driban, J., Kriska, A., McAlindon, T., Souza, R., Petersen, N., Storti, K., Eaton, C., Hochberg, M., Jackson, R., Kwoh, C., Nevitt, M., Suarez-Almazor, M. (2017). Is there an association between a history of running and symptomatic knee osteoarthritis? A cross-sectional study from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken), 69(2), 183-191. doi: 10.1002/acr.22939.
- Lo, G. H., Musa, S. M., Driban, J. B., Kriska, A. M., McAlindon, T. E., Souza, R. B., Petersen, N. J., Storti, K. L., Eaton, C. B., Hochberg, M. C., Jackson, R. D., Kwoh, C. K., Nevitt, M. C., & Suarez-Almazor, M. E. (2018). Running does not increase symptoms or structural progression in people with knee osteoarthritis: data from the osteoarthritis initiative. Clinical rheumatology, 37(9), 2497–2504. https://doi.org/10.1007/s10067-018-4121-3
- Khan, M., O’Donovan, J., Charlton, J. M., Roy, J. S., Hunt, M. A., & Esculier, J. F. (2021). The Influence of Running on Lower Limb Cartilage: A Systematic Review and Meta-analysis. Sports medicine, 10.1007/s40279-021-01533-7. Advance online publication. https://doi.org/10.1007/s40279-021-01533-7
- Bernard N. J. (2018). Growth factors respond to cartilage damage. Nature reviews. Rheumatology, 14(8), 444. https://doi.org/10.1038/s41584-018-0048-y
- Chew, J. (Host). (March 6, 2021). The Physio Matters Podcast [Audio Podcast]. Episode 87 – Wear Are We With Osteoarthritis With Professor Tonia Vincent.
- Uthman, O., van der Windt, D., Jordan, J., Dziedzic, K., Healey, E., Peat, G., et al. (2013) Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. BMJ; 347. doi: 10.1136/bmj.f5555
- Fransen, M., McConnell, S., Harmer, A. R., Van der Esch, M., Simic, M., & Bennell, K. L. (2015). Exercise for osteoarthritis of the knee. The Cochrane database of systematic reviews, 1, CD004376. https://doi.org/10.1002/14651858.CD004376.pub3
- McAlindon TE, Bannuru RR, Sullivan MC, et al. (2014) OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage, 22, 363–88.
- Skou, S., Pedersen, B., Abbott, J., Patterson, B., Barton, C. (2018). Physical activity and exercise therapy benefit more than just symptoms and impairments in people with hip and knee osteoarthritis. J Orthop Sports Phys Ther.;48 (6):439-447. doi: 10.2519/jospt.2018.7877.
- Luan, L., Bousie, J., Pranata, A., Adams, R., Han, J. (2020). Stationary cycling exercise for knee osteoarthritis: A systematic review and meta-analysis. Clinical Rehabilitation Nov 10;269215520971795. doi: 10.1177/0269215520971795
- Andriacchi, T. P., Favre, J., Erhart-Hledik, J. C., & Chu, C. R. (2015). A systems view of risk factors for knee osteoarthritis reveals insights into the pathogenesis of the disease. Annals of biomedical engineering, 43(2), 376–387. https://doi.org/10.1007/s10439-014-1117-2.
- Berenbaum, F. (2013) Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!), Osteoarthritis and Cartilage; 21(1): 16-21. https://doi.org/10.1016/j.joca.2012.11.012.
- Hunter, D. (2018) Osteoarthritis: time for us all to shift the needle. Rheumatology, (57), Issue suppl_4, Pages iv1–iv2. https://doi.org/10.1093/rheumatology/key065
- Wang, X., Hunter, D., Xu, J., Ding, C. (2015). Metabolic triggered inflammation in osteoarthritis. Osteoarthritis and Cartilage; 23(1):22-30. https://doi.org/10.1016/j.joca.2014.10.002.
- Benatti, F. B., & Pedersen, B. K. (2015). Exercise as an anti-inflammatory therapy for rheumatic diseases-myokine regulation. Nature reviews. Rheumatology, 11(2), 86–97. https://doi.org/10.1038/nrrheum.2014.193
- Hyldahl, R. D., Evans, A., Kwon, S., Ridge, S. T., Robinson, E., Hopkins, J. T., & Seeley, M. K. (2016). Running decreases knee intra-articular cytokine and cartilage oligomeric matrix concentrations: a pilot study. European journal of applied physiology, 116(11-12), 2305–2314. https://doi.org/10.1007/s00421-016-3474-z
- Helmark, I.C., Mikkelsen, U.R., Børglum, J. et al. (2010). Exercise increases interleukin-10 levels both intraarticularly and peri-synovially in patients with knee osteoarthritis: a randomized controlled trial. Arthritis Res Ther, 12,R126. https://doi.org/10.1186/ar3064
- Maurer, E., Klinger, C., Lorbeer, R., Rathmann, W., Peters, A., Schlett, C. L., Nikolaou, K., Bamberg, F., Notohamiprodjo, M., & Walter, S. S. (2020). Long-term effect of physical inactivity on thoracic and lumbar disc degeneration-an MRI-based analysis of 385 individuals from the general population. The spine journal : official journal of the North American Spine Society, 20(9), 1386–1396. https://doi.org/10.1016/j.spinee.2020.04.016
